Women’s Health
- Introduction
- Cervical Screen (Pap Smear)
- Breast Care
- Mammogram
- Polycystic Ovarian Syndrome (PCOS)
- Endometriosis
- Thrush
- Prolapse
- Urinary Tract Infection (UTI)
- Incontinence
- Female Genital Cutting (FGC)
- Menopause
- Helplines / Useful Information
Introduction

This article can help women understand more about their health and what they can do to be and stay healthy.
Right to care
- You have a right to understand your own health and to make informed decisions about your own body.
- All medical staff should communicate with you throughout your visit.
- You have the right to an interpreter and to ask that they be a woman.
- If you don’t know what is happening to you, you have a right to ask staff to stop and explain what is happening.
- You also have a right to say ‘no’ or to ask for more information before consenting to a treatment.
Information for this website sourced from: Cancer Council Victoria: Cervical screening is important for every woman, HPV Vaccine, Sydney Breast Cancer Foundation, Wikihow.com, Better Health Channel, BreastScreen Victoria, Health Direct: Endometriosis, Better Health Channel, Jean Hailes Foundation, Healthy WA, Continence Foundation of Australia, Menopause – Health Direct, The Women’s Hospital, The Menopause Society
Cervical Screen (Pap Smear)

Due to the recent changes to Australia’s Pap screen program, this information has been adapted from Cancer Council Victoria and HPV Vaccine.
Pap tests are now cervical screens. This new screening test looks for HPV (which causes almost all cervical cancers), not just abnormal cells (like the Pap smear test did). HPV is a virus that can cause some genital cancers in men and women. On 1 December 2017, Australia switched to a renewed cervical cancer screening program.
This new test means you will only need to have a screen every five years between ages 25-74.
In Australia, women from different cultural or language backgrounds are less likely to have regular cervical screening. It’s very important that all women, no matter what language they speak or how long they have been in Australia, have Cervical Screening
Information about Cervical Screening Tests and preventing cervical cancer is available in languages other than English here. You can ask your doctor or health professional about cervical screening, or call the Translating and Interpreting Service on 13 14 50 to speak to a Cancer Council nurse in your language.
Where to go for a Cervical Screen?
You may be able to complete your own cervical screen so speak to your doctor or women’s health specialist for more information.
If you have suffered sexual assault, having a cervical screen can feel scary and you may not want to be tested. Finding an experienced cervical screen provider is possible and you have a right to access care that makes you feel safe and respected.
Women who identify as LGBTQI+, Aboriginal and Torres Strait Islander women and women with disabilities often find it harder to access respectful, safe and informative care.
Accessing this care is your right and you deserve to be treated well at every appointment. You can find more information below and here about accessing services specific to your needs.
Cervical Cancer Vaccine
The vaccine “Gardasil” can prevent most HPV-related cancers.
The National HPV Vaccination Program is for girls and boys aged 12 to 13 years. It is important that anyone who has commenced the vaccination program to continue to receive all three vaccination doses.
Cervical Screening and Female Genital Cutting (FGC)
The experience of FGC can prevent some women from getting a cervical screening test. You may find it helpful to:
- Know that the appointment is private and confidential
- Take a relative or friend with you to help you feel more comfortable
- Ask for a female nurse or doctor
- Ask your nurse or doctor about the test before it happens
- Stop or pause the test at any time
- Ask for a sheet to put over you during the test
Breast Care

Breast cancer is the most common cancer in Australian women. One in nine women will have breast cancer by the age of 85 years. In Victoria, around 3,000 women are diagnosed with breast cancer each year.
In 2006 more than 660 Victorian women died from breast cancer, making it the second most common cause of cancer-related death in women after lung cancer.
Breast exam
You can do your own breast exams at home while lying flat on bed or when you are in the shower (see image below).
You are looking for any changes to your breast such as:
- Lumps
- Redness
- Pain
- Nipple leakage
- Swelling
- A change in size of one of your breasts that makes them uneven.
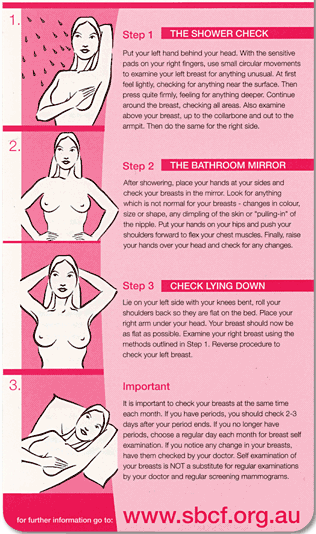
Image Courtesy of Sydney Breast Cancer Foundation
You can also ask your doctor or a trained nurse to give you a breast exam. They do this by massaging your breast and tissue around this area to feel for lumps.
If you or your doctor/nurse feels something abnormal you will be referred to have a mammogram (breast x-ray)
You may also have to have a small procedure called biopsy. In a biopsy, a specialist doctor will remove some breast tissue and have it tested to make sure the lump is not cancerous.
Follow this link to learn how to check your own breast.
Learn more here:
Mammogram

BreastScreen Victoria invites women aged 50-74 who do not have breast symptoms for a free breast screen (called a mammogram) every two years.
BreastScreen Victoria is a free service and you don’t need a doctor’s referral. Clinics are located all over Victoria, so you can attend one that is most convenient for you.
Early detection and treatment can reduce illness and death from breast cancer.
If you experience any breast symptoms or unusual changes, see your doctor without delay. You can book an online appointment at a clinic near you. They can arrange booking in your community group together and organise interpreters if you need them too.
There are even mobile breast screen vans that come to communities if you find it hard to access a clinic or want to go with some friends and get a screen together.
Learn more here:
Polycystic Ovarian Syndrome (PCOS)

Polycystic ovary syndrome (PCOS) is a hormonal condition which affects up to 1 in every 5 women in Australia
For you to be diagnosed with PCOS you need at least two out of the three symptoms:
- Polycystic ovaries seen on ultrasound scan
- Blood tests that show too much of a hormone called androgen and physical signs such as acne, too much hair on your face and/or body, or male pattern hair loss (i.e. balding)
- Irregular periods ovulation that suggest a menstrual cycle shorter than 21 days or longer than 35 days
The symptoms of PCOS can be treated individually and sometimes medications that contain synthetic hormones can help.
Having a healthy diet, exercising and keeping your weight at a healthy level is the best treatment for most women living with PCOS.
For more information you can download the AskPCOS app. PCOS App was developed by leading PCOS experts from around the world and co-designed with women with PCOS.
Learn more here:
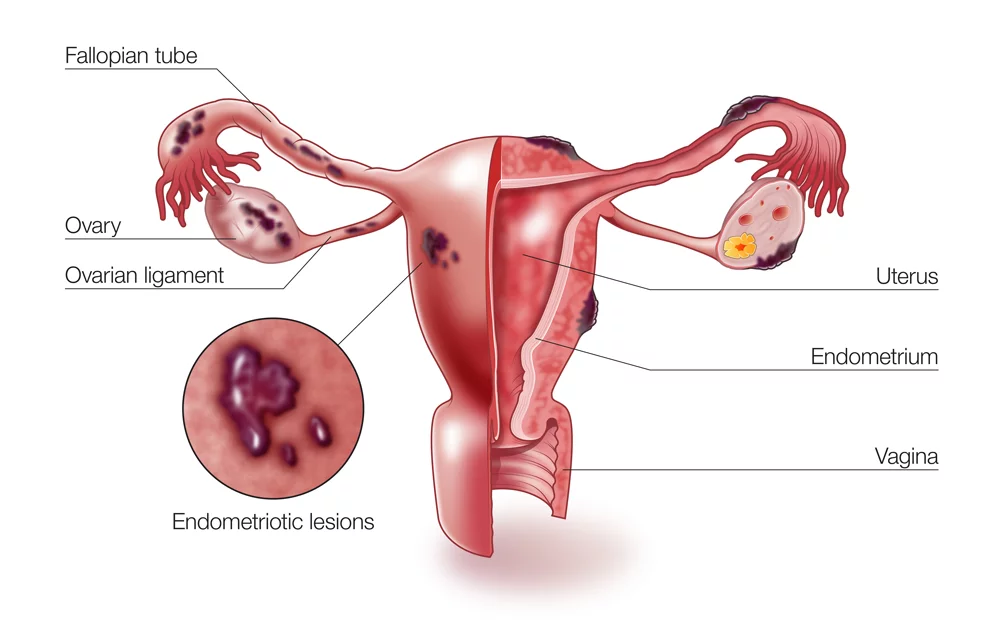
Endometriosis
Endometriosis is a condition in which cells similar to those that line the uterus – the endometrium – grow in locations outside the uterus.
Endometriosis may cause very painful periods and may reduce fertility, but there are a number of treatment options including pain relief, hormonal contraceptives and in some cases, surgery.
Signs and symptoms may include:
- Painful periods
- Pain with sex
- Pelvic pain
- Ovulation pain
- Pain in the lower back and thighs
- Bowel symptoms – pain using your bowel
- Bladder symptoms – pain when passing urine
- Reduced fertility
- Nausea and lethargy
- Premenstrual symptoms.
Chat to your doctor or women’s health nurse if you are worried you might have endometriosis.
Learn more here:
Thrush
Thrush is an infection caused when your vagina has too much of a naturally occurring bacteria called Candida albicans.
Thrush often happens after taking antibiotics, after you have been sick or during pregnancy when the immune system is weaker.
Most women get vaginal thrush at some point in their life.
Thrush can cause an itching or burning feeling (or both). Thrush can leave your vaginal and vulva area looking red and cause a white discharge
You can also have thrush in other parts of your body, such as the mouth and eyes
You should visit your chemist for a vaginal cream or tablets. You should also avoid having sex until after you have finished your thrush treatment
See your doctor if you have thrush more than twice during a single year
Learn more here:
Prolapse
A prolapse happens when one or more of the pelvic organs (bladder, bowel or uterus) drops down into the vaginal passage.
This may happen because the muscles in your pelvic floor have weakened over time, due to pregnancy or childbirth or in rare case, following a trauma.
A prolapse might cause:
- Constipation
- Incontinence or urinary retention
- Pain during sex
- Discomfort sitting down
- A feeling of heaviness in the vagina
Treatment is usually focused on pelvic floor exercises.
Some women may also need to take tablets to ease the symptoms or need surgery.
For more information, see your GP or women’s health specialist and visit the links below.
Learn more here:
Urinary Tract Infection (UTI)

A UTI is any infection to the urethra, bladder, ureters, or kidneys.
Anyone can have UTI, but some people are more at risk. Women who are sexually active and pregnant women are at increased risk of getting a UTI.
The symptoms of UTI can include:
- Burning when you pass urine
- A need to pass urine more than usual
- Passing only small amounts of urine
- Foul smelling urine
- Lower back pain
UTIs are diagnosed with a urine test and treated with antibiotics.
You may want to see your doctor or, if you think it is only a mild case, you may want to chat to you chemist first.
Learn more here:
Incontinence
Incontinence is when you can’t control when you need to pass urine or open your bowels (wee or poo)
For some women this can happen when you sneeze, laugh or cough.
There a many causes of incontinence, but pregnancy and childbirth increase your chances of experiencing both. This is because your muscles relax during pregnancy and childbirth and this can weaken and damage your pelvic floor.
Your risk of incontinence increases as you get older.
You can see your GP if you think you have incontinence but a physiotherapist can help strengthen your pelvic floor muscles. Some women may need more help than this e.g. surgery.
Incontinence is not something to be ashamed of.
You have a right to access care from health professionals who can treat you with respect and dignity.
Learn more here:
- Urinary Incontinence (The Women’s Hospital)
- Women (Continence Foundation of Australia)
- Incontinence and continence problems (Better Health Channel)
- Bladder incontinence (Jean Hailes)
Female Genital Cutting (FGC)
In some countries, girls’ genitals are cut as a rite of passage into womanhood. This is called female genital cutting (FGC) or female circumcision.
FGC can happen to a girl when she is very small or when she is about to enter puberty.
There are 4 types of FGC and this is based on how much of the genitals is removed.
- Type I: removal of the clitoral hood (the skin around the clitoris) with partial or complete removal of the clitoris
- Type II: removal of the labia minora (the inner lips that cover the vagina), with partial or complete removal of the clitoris and the labia majora (the large skin folds that cover the genital area)
- Type III: removal of all or part of the labia minora and labia majora, with the stitching of a seal across the vagina (called infibulation), leaving a small opening at the back for wee and menstrual blood and to have sex
- Type IV: other different things done to the female genitals, including pricking, piercing, cutting or cauterisation of the clitoris, cutting of the vagina, and introduction of herbs or corrosive substances
Not every girl or woman who has undergone FGC knows what type(s) she has experienced and some don’t even know that they have been cut.
The type of cutting may potentially cause pain or difficulty during your monthly period, when giving birth or having sex.
In Australia, it is illegal to perform female genital cutting or to send your child overseas to be circumcised.
If you are pregnant, you may have to have your cutting reversed during childbirth to make room for the baby. This is called deinfibulation. In Australia, the medical staff will not re-cut you afterwards as this is also against the law. If you don’t want to have this procedure done, you will need to have a caesarean-section
The reasons for FGC are different for every community. For some people it is seen as a family’s decision, an act of faith or a community tradition.
FGC is controversial throughout the world and may leave some women feeling ashamed if they have experienced it and others ashamed if they haven’t.
It is important that you speak to someone who won’t make you feel embarrassed, judged or ashamed for whatever decision you make.
You can discuss female cutting with a trained healthcare educator or a doctor/nurse who specialises in this area.
In Victoria, FARREP workers are experts in FGC. You can contact them on (03) 8345 3058.
Female Circumcision Booklet – For Communities, in Multiple Languages
The Women’s FGC and the Law in Victoria FGC (cohealth)
Menopause

Menopause is when a non-pregnant woman stops having her period for more than 12 months. This means that she can no longer get pregnant.
Menopause can be a slow process, and it might take a couple of years to complete.
The usual age for menopause is between 45 and 55. If a woman experiences menopause before the age of 40, it is called ‘premature menopause’. If she experiences these before the age of 45 it is called ‘early menopause’.
Menopause can cause side effects including:
- Hot flushes (feeling warm/hot suddenly, for no reason)
- Vaginal changes (dryness, irregular bleeding)
- Mood changes (sometimes you’ll feel sad, angry, happy or tired for no reason)
Some women need hormone replacement therapy (known as HRT) to manage the side effects.
Menopause can be a difficult time for some women and a relief for others.
Speaking to you GP or women’s health practitioner can help you work out how best take care of yourself during this change of life process.
Learn more here:
Useful Links
Pap test (cervical screen)
- Gardasil and the HPV Vaccine
- Cancer Council Screening Program
- Services that Family Planning NSW offers to people with disabilities
Breast Screen
- How to check your own breast
- Breast screening
- Breast screening fact sheets
- Make a booking for a breast screen
- Learn more about mobile screening
PCOS
- PCOS (Jean Hailes)
- Polycystic ovarian syndrome (Better Health Channel)
- Polycystic Ovary Syndrome (FPNSW
Endometriosis
Thrush
- Vaginal Thrush (Health Direct)
- Vaginal Thrush (Better Health Channel)
- Genital Thrush (Healthy WA)
Prolapse
- Prolapse and bladder weakness (Jean Hailes)
Urinary Tract Infection
- Urinary Tract Infection (UTI) (Better Health Channel)
- Urinary tract infection (UTI) (Health Direct)
- Urinary tract infections (UTIs) (NPS MedicineWise)
- Urinary tract infections (UTIs) (Jean Hailes)
Incontinence
- Urinary Incontinence (The Women’s Hospital)
- Women (Continence Foundation of Australia)
- Incontinence and continence problems (Better Health Channel)
- Bladder incontinence (Jean Hailes)
Female Genital Circumcision (FGC)
Menopause
- Videos (The Menopause Society)
- Menopause (Better Health Channel)
- Menopause (Jean Hailes)
- Health Direct
- Managing Menopause (The Women’s Hospital)
- Information Sheets (The Menopause Society)
Last reviewed: Jun 2022
