Labour And Birth
- Introduction
- Preparing for Birth
- Birth Support
- Signs of Early Labour
- The first stage of labour
- When to go to hospital
- Taking care of yourself in labour
- The second stage of labour
- Pushing
- The third stage of labour
- Forceps and vacuum delivery
- Caesarean Section
- Helplines/ Useful Information
Labour and Birth
Read this article to learn about your right to receive respectful maternity care.
You will also learn about how to prepare for birth, what to do during the three stages of labour and different ways of giving birth to your baby.
Right to respectful maternity care
- Your midwife and any other medical staff who are present should talk with you throughout your labour and birth.
- If you do not understand anything that is happening to you, you have a right to ask them to stop and explain what is happening.
- You also have a right to say no to care or to ask for more information before saying yes to any treatment.
- This is called informed consent.
- You have a right to an interpreter during your labour and birth.
- You can also request that the interpreter be a woman.

White Ribbon Alliance, Best Start: The Ontario Maternal, Newborn, and Early Childhood Resource Center The Women’s Hospital, Birth for Humankind.
Images and videos sourced from Catie Atkinson (Spirit y Sol), 7activestudio, Balkanopathy, Prenatal Education Key Messages for Ontario and Baby Centre
Preparing for Birth
- Most women give birth between 38 and 42 weeks of pregnancy.
- If you have your baby before this time, your baby may need to stay in the special care nursery (SCN) or newborn intensive care centre (NICU) for more specialised care.
- Some women may feel like they are having contractions from 34 weeks of pregnancy, but most do not go into labour until 38 weeks or later.
- These contractions are often called tightenings and may be uncomfortable, but are not usually painful.
- In early labour, your body is preparing for birth. During this time, you can:
- stay at home for as long as you can
- have regular snacks to keep up your energy
- rest as much as possible; if it is night time, you can try to sleep
- try relaxing in a bath or a shower
- go to the toilet regularly
Here is a list of things to consider taking to the hospital for you and your baby, courtesy of Birth for Humankind.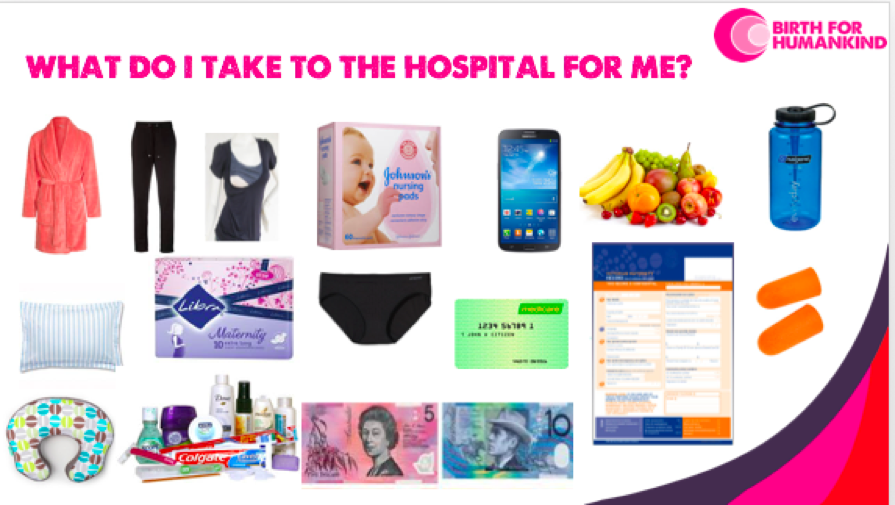
Learn More
Birth Support
- You have a right to have a support person with you during your labour. This may be your partner, a family member or friend, or a doula (trained birth companion but different to a midwife).
- Professional doulas charge fees for their service.
- In Victoria, Birth for Humankind offers a free doula service for women who with financial difficulties and who meet at least one following criteria:
- at risk of or experiencing perinatal depression and anxiety
- under 25 years of age
- experiencing or at risk of homelessness
- is a refugee, asylum seeker or newly arrived migrant (within 5 years)
- has a history of mental illness, drug and alcohol misuse, trauma or abuse issues
- is Aboriginal or Torres Strait Islander
- lacking a birth support person
- In Victoria, Birth for Humankind offers a free doula service for women who with financial difficulties and who meet at least one following criteria:
- You can make a referral for yourself or someone else by visiting Birth for Humankind.

Signs of Early Labour
- When you go into early labour, you may notice:
- a blood-stained, yellow or white discharge on your underwear (called a “show”)
- lower back pain
- period-like pain that comes and goes but may not be consistent
- loose bowel motions/diarrhoea
- a sudden gush or a slow leak of fluid from the vagina
- this is probably your waters breaking (also called your ‘membranes rupture’)
- these ‘waters’ should be clear or slightly pink
- a greenish or brown colour on your underwear or pad could mean there is a problem so you should visit you maternity centre immediately if this happens
Your midwife or doctor should discuss with you your birth plan, if you have one, towards the end of pregnancy.
If your pregnancy is low risk, they will encourage you to labour at home as long as you feel safe and comfortable to do so.
The first stage of labour
- Labour pains are contractions that come like waves, starting small, building to a peak and then falling away again.
- Contractions will come more often as you progress in labour.
- They will make you want to moan and make noises that may seem unusual, but this is normal.
- When your contractions are about a minute long and come every 3-4 minutes, you should go to the hospital.
- Many women do not like touching or talking during a contraction and just try to sleep in between them.
- Below are some positions that might help you during labour.
- The more you move around and sway your hips, the easier it is for your baby to move down and for labour to progress.
- At the end of the first stage of labour:
- you will start feeling a little more restless (it will be hard to sit still or lie down)
- you will feel tired and your pain will become stronger
- as you move closer to the second stage, the time between each wave will be shorter.
- You should go to the hospital when there is less than 3-5 minutes between each wave.

Image courtesy of: Best Start: The Ontario Maternal, Newborn, and Early Childhood Resource Center
When to go to hospital
- It’s OK to not be sure if labour has started or not.
- Sometimes it might feel like you are in labour for a couple of minutes or hours and then everything will slow down. This doesn’t necessarily mean something is wrong.
- Call the midwife or maternity ward at your local hospital if you are unsure.
- The midwife will:
- ask about your symptoms
- listen to how you breath through a few contractions
- help you to feel safe to stay home a little longer if it is too early to come in
- The midwife will:
- Your midwife will also ask you;
- how and where you feel your contractions
- how often the contractions come
- how long they last
- This helps the midwife to know how your labour is progressing and plan for when you may need to come in later.
- If your midwife thinks active labour has started (called “established labour”) they will ask you to come to the hospital.
- Depending on your situation, it is better to stay at home if you are not in established labour.
- You should call your hospital if your contractions are regular, you can’t talk through them, you start bleeding, or your waters break.
- Women often feel better at home in the early stages of labour.
- If this is OK by you and your midwife, you should rest at your home for as long as you feel safe and comfortable to do so.
- Your doctor or midwife should discuss pain relief in labour with you towards the end of your pregnancy.
- You have a right to ask for or say no to medication in labour.
- You have a right to say no to pain relief.
- Some common pain relief options are:
- massage and acupressure
- TENS machines
- water immersion (e.g. bath/shower)
- sterile water injections (these are placed in your lower back)
- nitrous oxide gas (also called “gas and air”)
- morphine or pethidine injection (depending on the hospital policy)
- epidural block
Learn More
Taking care of yourself in labour
For many first-time mothers, labour can take between 6 and 20 hours before it’s time to push.
Pushing can also take a few hours, so it is important to take care of yourself and rest as much as possible.
- You can try:
- to concentrate on your contractions and rest in between each one
- to let go and allow your body to do what it needs to do
- different positions – sitting, standing or walking
- a cold face washer if you get too hot, this can be very soothing
- a bath or shower to help you to relax and to manage the pain
- Remember to keep drinking water or sucking ice and to rest as much as you can.
- Some of the positions below might help you during labour.
- The more you move around and sway your hips, the easier it is for your baby to move down and for labour to progress.

Labour and Birth Positions Chart by Catie Atkinson (Spirit y Sol) and can be purchased here
The second stage of labour
- The second stage of labour starts when the cervix (the opening of the uterus) reaches 10cm and ends when your baby is born.
- In the second stage you may experience:
- longer and stronger contractions, with a different break period in-between compared to earlier in labour
- increased pressure in your bottom
- the desire or need to push down through your bottom
- shaky legs
- feeling sick or vomiting
- stretching and burning feelings in your vagina/vulva
- Most women are worried about tearing along their perineum (the skin between the vulva / vaginal opening and anus /rectum) during childbirth.
- Your midwife or doctor can help reduce tearing by guiding you through the pushing stage and applying warm compresses against your perineum towards the end of the second stage.
- If you do not want them you can ask them to stop.
- Not all tearing requires stitches and your midwife and doctor will do their best to reduce the risk of you tearing.
- In some hospitals staff may offer an episiotomy which is when they use special scissors to make your birth opening bigger. This will require stitches after you have had your baby.
- Episiotomy is no longer recommended as a routine procedure
- You can decline this both before or during childbirth.
- If it is an emergency the staff should still ask your consent to perform an episiotomy.
The following video can help you to better understand the experience of labour and birth.
Pushing
- When you feel the need to push, it can be overwhelming.
- The pushing phase is different for each woman, but can last for up to 2-3 hours.
- It is usually shorter if you have had push out another baby previously
- When it’s time to push you may also feel:
- pressure and a strong need open your bowels (do a poo)
- the baby’s head moving down
- stretching and burning in your vagina
- The best thing you can do during this phase is to try and breathe deeply, relax and follow your body’s need to push
- Trust and listen to your midwife or doctor who will guide you
The third stage of labour
- The third stage begins after your baby is born and finishes when your body pushes out the placenta.
- This usually happens within 5-30 minutes after birth.
- In the third stage, you may have:
- more contractions to push the placenta down and out of your vagina
- a feeling of fullness in your vagina or like you need to open your bowels (do a poo)
- In an “active third stage” the midwife or doctor will give you an injection in your thigh as the baby’s shoulders are being born.
- This is a synthetic form the oxytocin hormone (called Syntocinon or Pitocin) and helps the placenta come away from the uterus.
- They will then apply gentle but firm traction (pressure at an angle) on the umbilical cord to deliver the placenta.
- They may ask you to help by gently pushing down with each contraction.
- You can cuddle and breastfeed your baby immediately after birth and during the delivery of your placenta.
- Some people like to see or keep their placenta.
- Let your midwife or doctor know if you would like to do this and they can arrange to put it into a special container to take home.
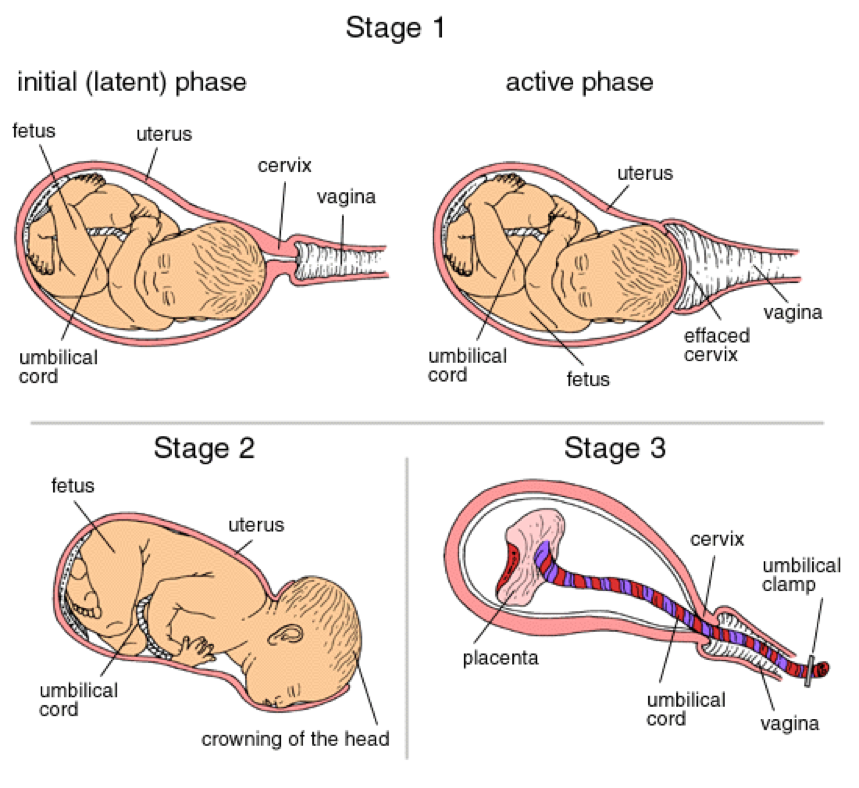
Image courtesy of Balkanopathy
Forceps and vacuum delivery
- Sometimes during the end of the second stage, you or your baby may get too tired to keep pushing.
- If your baby’s position is making pushing difficult or your baby’s heart beat drops and doesn’t return to normal, your doctor may ask you for consent to use forceps or a vacuum (also called a “ventouse”).
- Your doctor may also need to make a cut along the birth passage, called an episiotomy.
- This gives your baby more room to come out but is not routine and they should always ask you before they do it.
- Most women get some grazes or small tears during birth.
- First and second-degree tears heal better than episiotomies but if your midwife or doctor is worried the tear might be bigger then they may ask to do an episiotomy.
- It is your right to ask questions and find out if there are other options.
- If you don’t understand what is happening, you can ask for an interpreter or ask your doctor to slow down and explain things more clearly.
- Below are some questions that you might want to think about before you decide.
- You can ask your midwife or doctor about this during your pregnancy, if you are nervous or do not understand anything.
Remember, it is your right to understand everything that is happening to you, your body and your baby throughout this time.
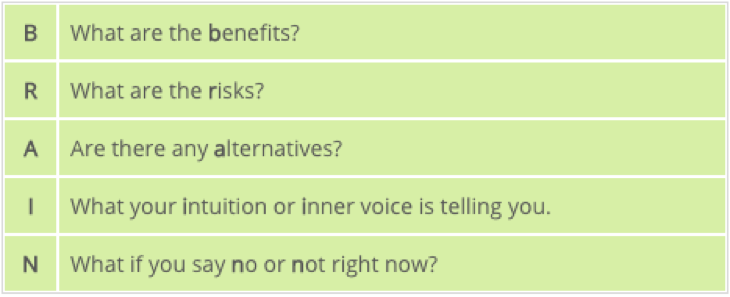
Image courtesy of: Prenatal Education Key Messages for Ontario
Caesarean Section (C-section)
- Some babies are born by caesarean section (C-section).
- This can be an emergency during or before labour if there is a complication with you or your baby or it may also be something you choose to do in advance (this is called an “elective C-section”).
- You should not feel judged for this decision.
- If you wish for C-section, you will need to discuss this with your doctor in advance.
- Elective C-sections are usually done around 38-39 weeks if your pregnancy is normal to reduce the chance of you going into labour first.
- You can breastfeed your baby after a C-section and you can ask for immediate skin to skin and cuddles.
- Having a C-section once does not mean you automatically have to have another one in future pregnancies
- You should discuss this with your doctor as a future vaginal birth after caesarean (VBAC) depends on a number of other factors too.

Image courtesy of: Baby Centre
Last reviewed: Jun 2022

