Complications
- Introduction
- Miscarriage
- Ectopic Pregnancy
- Gestational Diabetes Mellitus (GDM)
- Pre-Eclampsia
- Pre-term Labor
- Bleeding in Pregnancy
- Breech
- Perinatal Depression & Anxiety
- Helplines/ Useful Information
Complications of pregnancy

Read this article to learn more about possible complications in pregnancy.
You will also learn about miscarriages, ectopic pregnancies, gestational diabetes mellitus, pre-eclampsia and perinatal depression and anxiety.
Information for this page was sourced from SANDS, World Health Organization, Mercy Health Werribee, Royal Women’s Hospital, Raising Children Network, Victorian Agency for Health Information, King Edward Memorial Hospital, TIS National, Beyond Blue, Reach Out, PANDA and Health WA
Miscarriage
- A miscarriage happens when a pregnancy stops growing and the pregnancy tissue that would have become the baby passes out of the woman’s body.
- A miscarriage is not your fault and you can ask for help if you are feeling sad or disappointed.
- SANDS is an independent organisation that provides support for newborn death, stillbirth and miscarriage. You can call them on 1300 072 637.
- Facts:
- 1 in 3 women will experience a miscarriage at some point in her life.
- This can be a very sad and emotional time for a woman and her family.
- This is a common experience and you usually you can’t prevent it.
- Having one miscarriage does not increase your risk of another miscarriage.
- You should call or visit your doctor if you feel you are having a miscarriage (if you are having a lot of pain and/or are bleeding).
- Your doctor may ask you to wait until the bleeding stops.
- Some women may need to take medication or have surgery to remove the blood clots from their uterus (womb).
- The World Health Organization recommends you wait at least 6 months to reduce risks to you and your future pregnancy
Learn More
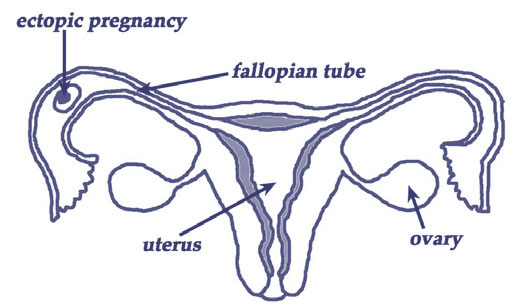
Ectopic Pregnancy
- An ectopic pregnancy happens when the baby starts to develop outside the womb.
- This usually happens in the fallopian tube (see below).
- This type of pregnancy cannot continue and you will need immediate surgery to remove the pregnancy tissue and affected fallopian tube.
- This will not affect your other fallopian tube and you can still get pregnant in the future.
- If you have an ectopic pregnancy, your doctor will ask you to have an ultrasound early in future pregnancies.
- This is to make sure that it doesn’t happen again.
Image courtesy of: Department of Health WA
Learn More
Gestational Diabetes Mellitus

Gestational diabetes mellitus (GDM) is a type of diabetes that develops during pregnancy.
- GDM develops when your body has trouble controlling sugar levels in your blood during pregnancy.
- GDM increases your risk of developing Type 2 diabetes later in life.
- You will have a blood test for GDM around 28 weeks into your pregnancy.
- You have a risk of developing GDM if you:
- have family history of diabetes
- you are overweight or obese
- have polycystic ovarian syndrome (PCOS)
- have history of GDM in previous pregnancies
- People with risk factors may need to have a test for GDM earlier in pregnancy.
- During the test, you will have be asked to have a blood test before and after having a sugary drink.
- You will be asked to sit still for 1-2 hours between these blood tests.
- If you test positive for GDM, your doctor will ask you to check your blood glucose level with a finger prick test before and after meals until your baby is born.
- Your doctor, midwife or diabetes educator will encourage you to increase you physical activity like taking a walk twice a day or going for a regular swim.
- Learning about healthy foods and managing your diet now will help you continue to take care if yourself after you have your baby.
- Some women may also have to take a medicine called insulin every day.
- By having regular check-ups and controlling your blood sugars, you can have a healthy pregnancy and birth.
- This will also help your baby’s health too.
- After your baby is born, your GDM will get better and your blood sugar will return to normal levels.
- Your doctor will ask you to have blood test again around 6 weeks after you give birth.
- If you have GDM once, you have an increased risk of having GDM in future pregnancies but you can reduce this risk by having a healthy diet and exercising regularly between pregnancies.
Learn More
Pre-Eclampsia

Pre-Eclampsia is a condition that some women develop usually towards the end of pregnancy or immediately after giving birth.
It affects the mother’s blood circulation, kidneys, liver and brain and can affect the blood flow to the baby too.
- You have an increased risk of developing pre-eclampsia if you:
- are having your first baby or if you had pre-eclampsia in a previous pregnancy
- are overweight or obese (BMI >30)
- have family history of pre-eclampsia (e.g. your mothers or sisters had it)
- have high blood pressure already
- have diabetes, kidney disease or lupus
- Symptoms
- Women with pre-eclampsia may experience:
- high blood pressure
- this is why your midwife or doctor checks your blood pressure at each antenatal appointment
- sudden swelling of the face, hands or legs
- protein in the urine
- this is why your midwife or doctor may test this at each antenatal appointment
- blurry vision
- you may see sparkles, stars or bright lights
- a slowing down of your baby’s growth
- this is why your midwife or doctor measures your tummy at each antenatal appointment
- high blood pressure
- Women with pre-eclampsia may experience:
- Treatment:
- If you have high blood pressure during pregnancy, your doctor may give you medication to to lower this and increase your number of antenatal visits
- If you develop pre-eclampsia, you will be admitted to hospital for monitoring and may have to deliver your baby earlier than their due date.
- Pre-eclampsia can get dangerous very quickly
- If pre-eclampsia is not treated, you may have seizures (also called “fits”) and this can be life-threatening for you and your baby.
- It is important to contact your doctor or midwife if you have any of the symptoms listed above.
- If pre-eclampsia is not treated, you may have seizures (also called “fits”) and this can be life-threatening for you and your baby.
Learn More
Pre-term Labor
Preterm labor is when you start having signs of labor before 37 weeks.

- The signs of labour are:
- contractions (painful, regular tightening of the utersu)
- feeling more pressure in the lower part of pelvis, especially around your bottom (like you need to open your bowels)
- fluid or blood coming from the vagina
- If you have any of these symptoms before 37 weeks, contact your midwife or go to the hospital immediately.
- Your baby may need extra help with breathing, feeding and staying warm if they are born before 37 weeks.
Learn More
Bleeding in Pregnancy
- Some women experience bleeding during their pregnancy.
- Bleeding during pregnancy is not normal but it does not mean that you are definitely having a miscarriage or going into labour.
- Depending on the amount of bleeding, your doctor may ask you to have more ultrasounds or be admitted to hospital for closer monitoring.
- You may need a blood transfusion or iron supplements.
- Your baby may need to be born earlier than their due date
- This bleeding may be because the placenta or blood vessels in the baby’s umbilical cord are close to, or covering the cervix (i.e. the opening of the womb).
Placenta praevia
- Towards the end of your pregnancy, the placenta will move up the wall of the uterus but this may not be high enough to allow you to have a vaginal birth or stop the risk of bleeding.
- This is called a placenta praevia.
- There are four levels of placenta praevia:
- Stage I: Low Lying – placenta is close to cervix
- Stage II: Marginal – placenta is next to cervix
- Stage III: Partial – placenta is covering part of the cervix
- Stage IV: Complete – placenta is covering the whole cervix
- There are four levels of placenta praevia:
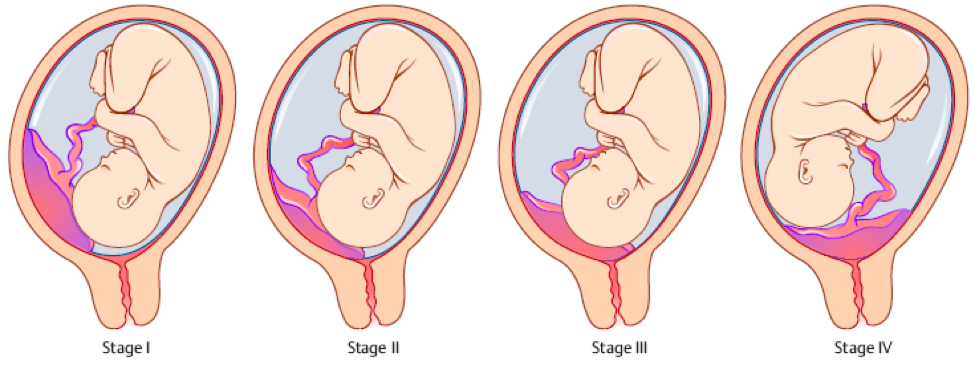
If your placenta is too close to the cervix, you may need to have a cesarean section (C-section).
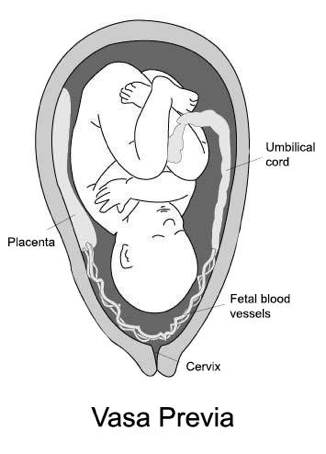
Vasa praevia
- Vasa praevia is a condition when the blood vessels inside the umbilical cord or placenta cross or lie near the cervix.
- Women with vasa previa may have:
- bleeding
- cord prolapse (where the cord enters the cervix before the baby’s head does. This is a medical emergency requiring immediately birth of the baby.
- Women with vasa previa may have:
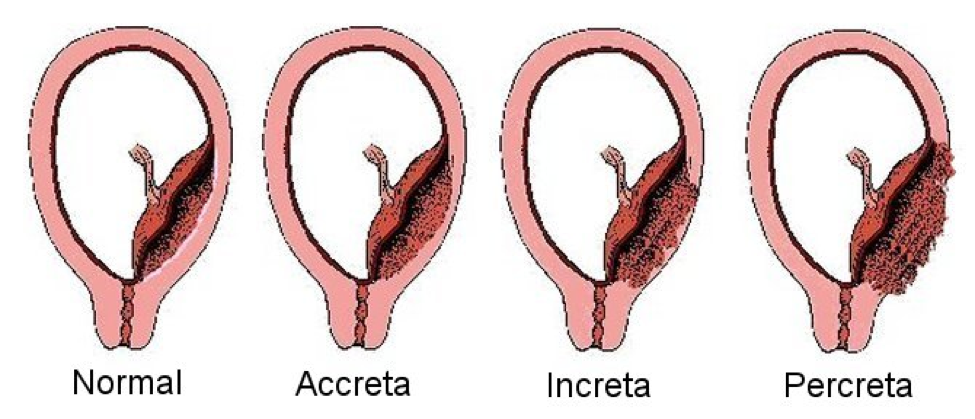
- Sometimes the placenta grows too deeply into the uterine wall.
- This is known as placenta accreta, placenta increta or placenta percreta (depending on how deep into the uterine wall the tissue grows).
- If you have any of these conditions, your doctor will advise you to give birth by C-section.
Placental abruption
- Placental abruption happens when the placenta separates early from the uterus during pregnancy or labour.
- This will also cause bleeding.
- Placental abruption is an emergency and your doctor will need to deliver the baby C-section.
- You may also need to stay in hospital longer or have a blood transfusion.
Breech
- Babies move around in your uterus throughout pregnancy.
- Sometimes they sit with their head under your rib cage and their bottom or feet towards the opening of your uterus.
- This position of the baby is called breech.
- Sometimes they sit with their head under your rib cage and their bottom or feet towards the opening of your uterus.
- The head of your baby should be facing down towards the end of your pregnancy.
- This position is called cephalic and is the best position for a vaginal birth.
- If this happens, your doctor will likely recommend birth by caesarean section (C-section).
- In Australia, there are few doctors who will offer support for a breech vaginal birth but some will depending on the exact position of the baby (see image below) and other risk factors.

Image courtesy of: Victorian Agency for Health Information
- Some doctors also offer a procedure called “external cephalic version”.
- This means your doctor will try to turn the baby around in the last few weeks of your pregnancy.
- They will do this with the help of an ultrasound and move their hands across your abdomen (or tummy) and try to turn the baby around from the outside.
- This means your doctor will try to turn the baby around in the last few weeks of your pregnancy.
Learn More
Perinatal Depression & Anxiety

It is common to experience some sadness, stress or feelings of fear or frustration during pregnancy or after the birth of your baby.
It may be difficult to know if this is normal or a sign that you may have depression or anxiety.
- Many mothers don’t ask for help because they believe that having a baby should only be a happy occasion. Some women may also fear other people will judge them.
- It’s OK to ask for help if you have feelings of sadness or worry that lasts more than a few days or if you have been feeling this way for weeks, months or even years.
- Your midwife, MCH nurse or doctor may also notice signs of depression or anxiety and they may ask you to answer some questions on a form.
- This form is called the Edinburgh Postnatal Depression Scale (EPDS) and you would have filled it out during one of your first antenatal appointments also.
- Your doctor or nurse may also have asked you to fill out the form in later pregnancy.
- No one has the right to take your baby away from you just because you are sad or worried.
- There are programs that can help you feel better and help you bond with your baby if this is something you are having trouble with.
- Some programs may help request you stay overnight at their centre and help you care for your baby as you get better. This is often called a “mother-baby unit”.
- There are programs that can help you feel better and help you bond with your baby if this is something you are having trouble with.
- You have a right to ask for help and feel better.
- Asking for help early on can make you feel better sooner and make your pregnancy and motherhood a more enjoyable experience.
PANDA has a list of signs that might suggest you or someone you know has perinatal depression or anxiety here. They include:
- Feeling sad, low, or crying for no obvious reason
- Persistent, generalised worry, often focused on fears for the health or wellbeing of your baby
- Being nervous, ‘on edge’, or panicky
- Being easily annoyed or irritated
- Withdrawing from friends and family
- Difficulties sleeping, even when your baby is sleeping
- Abrupt mood swings
- Feeling constantly tired and lacking energy
- Physical symptoms like nausea, vomiting, cold sweats, lack of appetite
- Having little or no interest in the things that normally bring you joy
- Fear of being alone or with others
- Finding it difficult to focus, concentrate or remember
- Increased alcohol or drug use
- Panic attacks (racing heart, palpitations, shortness of breath, shaking or feeling physically detached from your surroundings)
- Developing obsessive or compulsive behaviours
- Thoughts of death, suicide or harming your baby.
- There are also many other symptoms not listed here. If you or someone close to you experiences any symptoms or feelings that worry you for two weeks or more, please seek support.
- PANDA has been supporting individuals and families to recover from perinatal anxiety and depression for decades.
- PANDA also has resources in multiple languages here.
- You can call for yourself or someone you know if you have concerns about their mental health or wellbeing. PANDA‘s National Helpline is open Monday to Friday 9am – 7.30pm AEST/AEDT), call them on 1300 726 306. Tell them if you need a translator and PANDA will call you back with one from TIS National if you need.
Learn More
- Understanding perinatal depression and anxiety (beyondblue)
- Self-help for anxiety
- PANDA
- Edinburgh Postnatal Depression Scale (EPDS)
- St John of God Mother Baby Unit
- Masada Baby Unit
Links:
- Early Pregnancy Clinic (Miscarriage) (Mercy Health Werribee)
- What happens after a miscarriage (Royal Women’s Hospital)
Ectopic pregnancy
Gestational diabetes mellitus
Preterm labor
Perinatal Depression & Anxiety
- PANDA – Perinatal Anxiety & Depression Australia
- Edinburgh Postnatal Depression Scale (EPDS)
- St John of God Mother Baby Unit
Last reviewed: Jun 2022